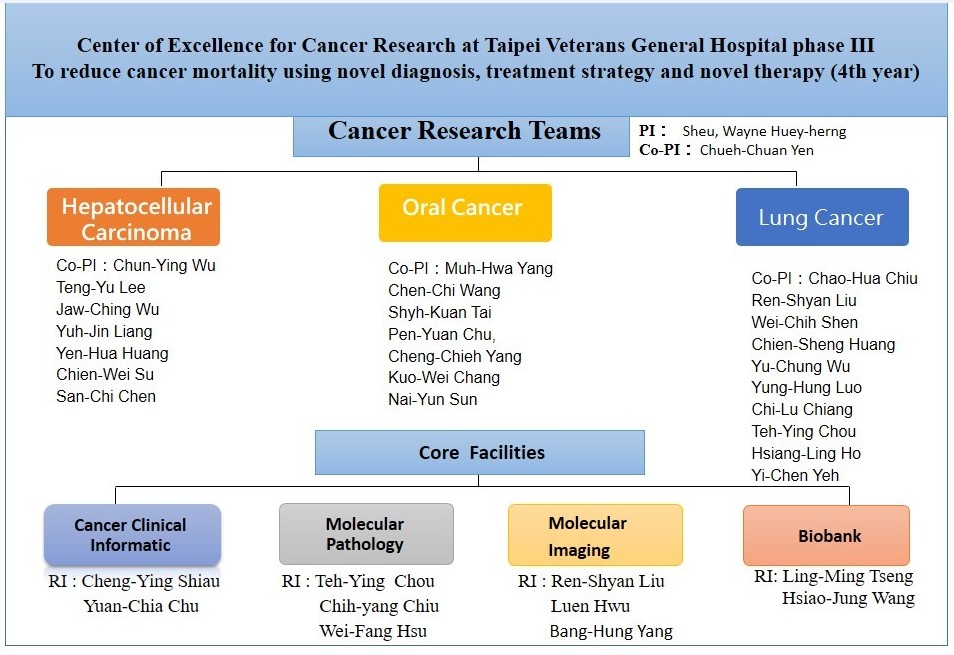
Taipei Veterans General Hospital jointed the project "Phase III Cancer Research Project: Reduce Cancer Mortality with New Diagnosis Methods, Treatment Strategies and Treatment Methods" of the Ministry of Health and Welfare during 2018-2021. This program is implemented by the Center of Excellence for Cancer Research of our hospital, with the former dean Wayne Huey-herng Sheu as the moderator, and Dr. Chueh-Chuan Yen assisting in the implementation. The research mainly focuses on the three types of cancer: liver cancer, oral cancer, and lung cancer. There are also four core facilities and teams supporting cancer research, including clinical cancer information system, molecular pathology laboratory, biomedical image analysis laboratory, and biobank. This project integrated clinical and translational exploration, as well as established multi-center, inter-institution and cross-field cooperation to conduct the research. Hopefully this project could achieve the goal of reducing cancer mortality and incidence.
Following are some important results
Liver Cancer Team
1. Studying the risk of liver failure and death in patients with chronic hepatitis B after stopping the antiviral drug
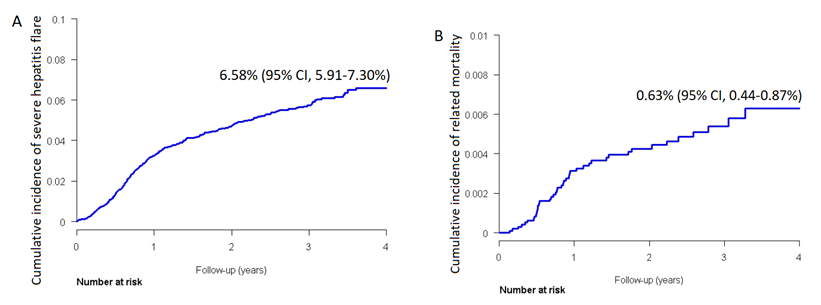
We analyzed the information of 10,192 patients with chronic hepatitis B obtained from Taiwan's National Health Insurance Research Database (NHIRD). For these patients, we found that after antiviral drugs were discontinued, the four-year cumulative incidence of liver failure was 6.58%. Male sex, liver cirrhosis, and a history of liver decompensation were risk factors. In the meantime, after stopping the antiviral agents in these patients, the four-year cumulative mortality rate was 0.63%. Age, liver cirrhosis and hypertension were risk factors. The results of this study suggest that anti-viral drugs should be continued in patients with chronic hepatitis B to avoid the risk of liver failure and death.
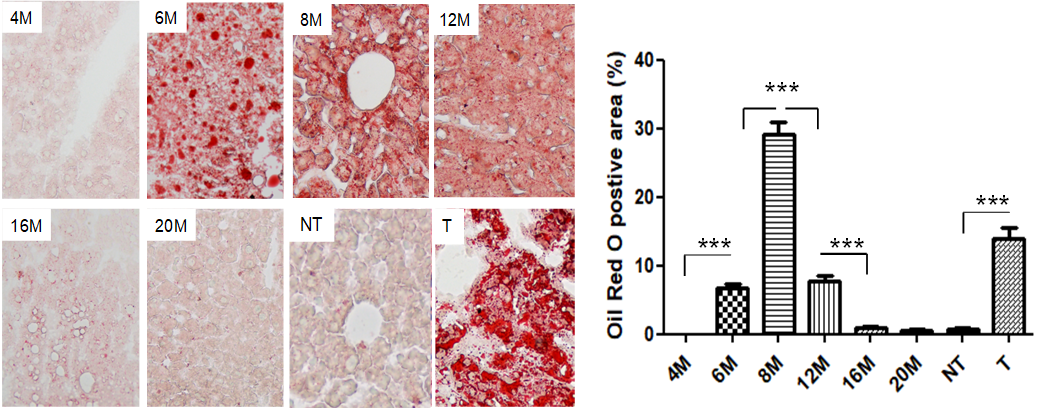
2. Tenofovir (TDF) treatment of the hybrid of transgenic mice of HBV and single copy miR 122 mice (D14/miR-122+/-) with high viral load, normal ALT and high incidence of HCC
(1) The dynamic change of fatty liver evolution over time among D14/miR-122+/- transgenic mice. Fatty liver could be found in the liver tissue of 6-month-old mice.
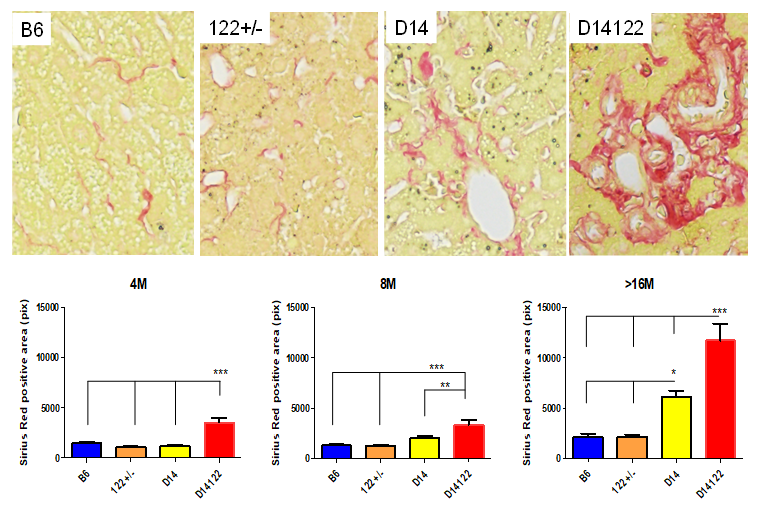
(2) Comparison of liver fibrosis among the different strains of mice。Liver fibrosis could be found in HBV/miR-122 +/- mice older than 16 months.
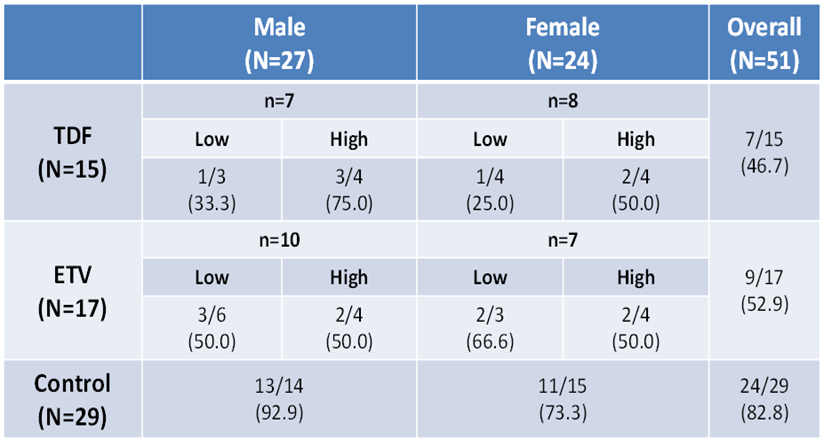
(3) Exploring the effect of antiviral drugs on the prevention of liver cancer in D14/miR-122+/- transgenic mice. Antiviral therapy (Entecavir, ETV; Tenofovir, TDF; or placebo) was prescribed when these mice were 6 months old, and the incidence of liver cancer was studied when they were 22 months old. Study showed that the chances of liver tumor development, in comparison with mice not receiving antiviral treatment (82.8%), were significantly lower in those receiving anti-viral therapy (TDF 46.7%, p=0.013,ETV 52.9%, p=0.03).
3. The mechanism and treatment strategy of molecular target therapy for advanced liver cancer
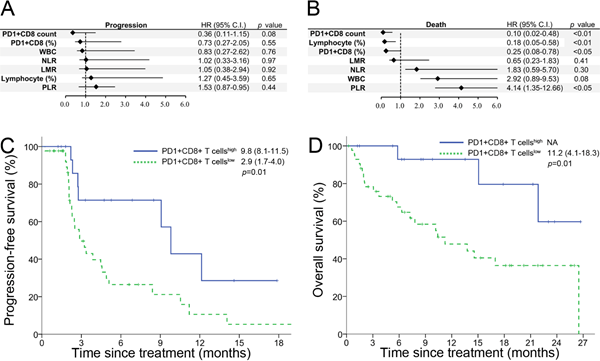
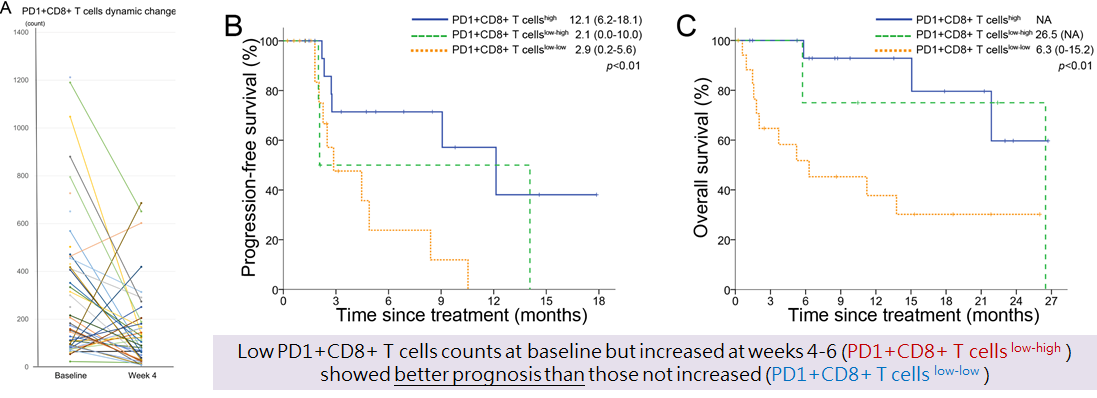
(1) High PD1+CD8+ T cell count can predict longer PFS and OS
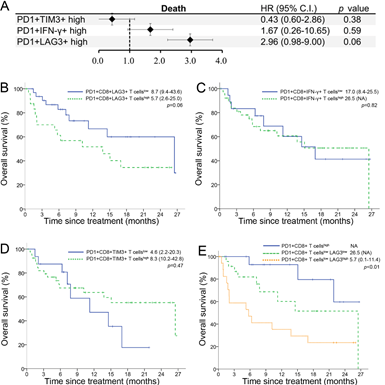
(2) High LAG3+ as a predictor of poor prognosis with immunotherapy
(3) Analysis of the changes in the number of PD1+CD8+ T cells after treatment shows that the markers predicting best prognosis is PD1+CD8+ T cells(high), followed by PD1+CD8+ T cells(low->high), and the worst is PD1 +CD8+ T cells(low->low)
Oral cancer team
1. Targeting CD73 enhances the antitumor effect of anti-PD-1 therapy in cetuximab resistant OSCC
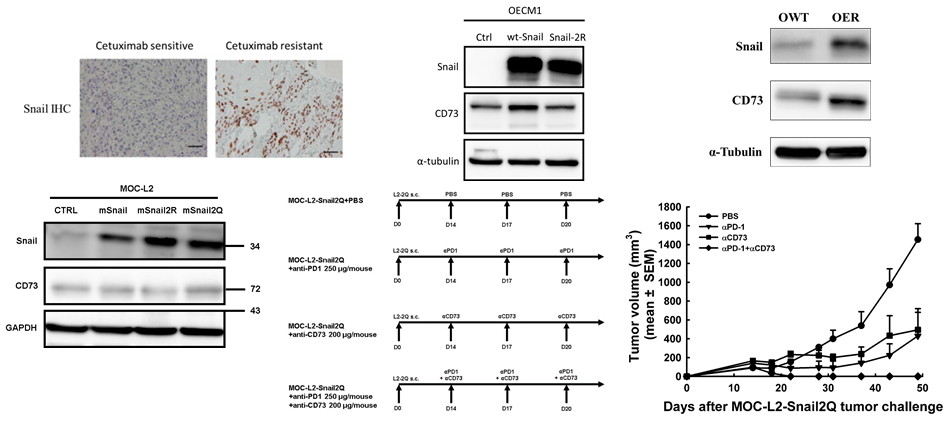
(1) The expression of Snail in the tumor specimens of oral cancer patients with drug resistance to cetuximab was significantly higher than those without. Acetylated Snail positively regulates the expression of CD73 in oral cancer cells. The expression levels of Snail and CD73 in cetuximab-resistant oral cancer cell lines were higher than those in non-drug-resistant ones.
Anti-CD73 can enhance the therapeutic effect of anti-PD-1 in acetylated Snail syngeneic mouse oral cancer model
2. Reduced STAT1-mediated immune checkpoint inhibitor resistance in cetuximab resistant HNSCC
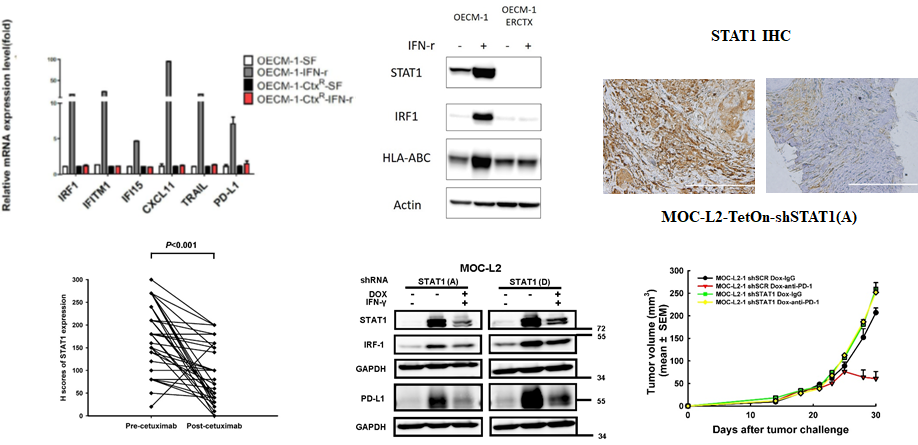
(1) cetuximab-resistant oral cancer cells respond poorly to IFN-γ
(2) Decreased STAT1 protein may be responsible for the poor response of cetuximab-resistant oral cancer cells to IFN-γ
(3) Analysis of 38 pairs of head and neck cancer patients before and after cetuximab treatment showed that the expression of tumor STAT1 protein in patients with cetuximab resistance was significantly reduced compared with that before treatment
(4) The syngeneic mouse oral cancer cells do not respond to anti-PD-1 treatment when conditional knockdown STAT1
3. Development of novel chemo-preventive strategies by exploiting hypomethylation in oral precancerous and cancerous lesions
(1) DNA hypomethylation, occurring in extensive non-coding regions in precancerous and cancerous lesions, is highly correlated with the occurrence and progression of cancer. Hypomethylation is induced by the high oxidative stress (ROS) of the cells produced by the chronic stimulation of carcinogens, which is related to the consumption of S-Adenosylmethionine (SAM) derived from methyl groups.
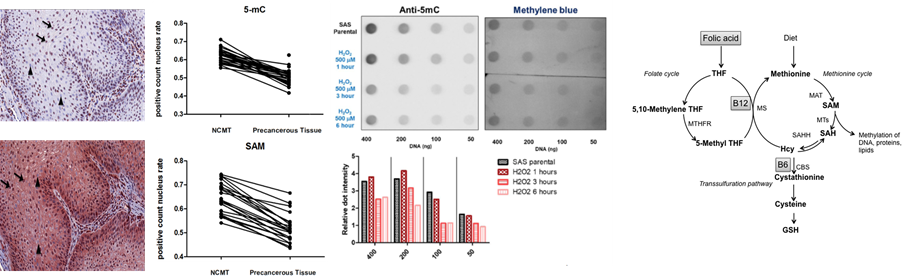
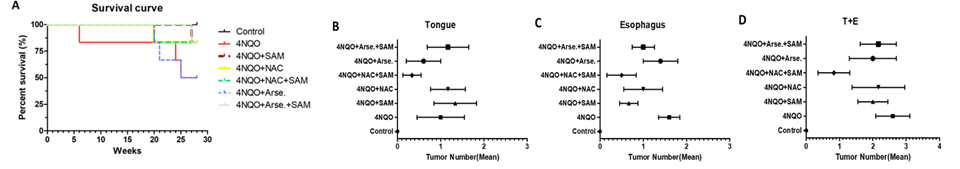
(2) Using the mouse model of 4NQO oral carcinogenesis to explore the chemoprevention strategy for oral cancer combined with SAM and ROS inhibitor N-Acetyl-L-cysteine (NAC)
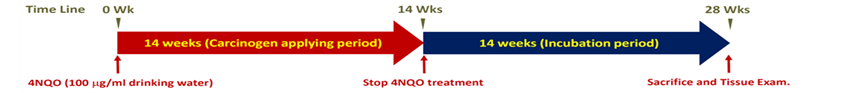
We then explored the possible chemo-preventive effect for oral cancer of SAM or NAC in mouse model using different combinations of supplements. At 28 weeks, the mice were sacrificed to measure the number of cancers in the oral cavity and esophagus. As shown in Figure D, the group given NAC and SAM at the same time had the least number of tumors in each group.
Lung Cancer Team
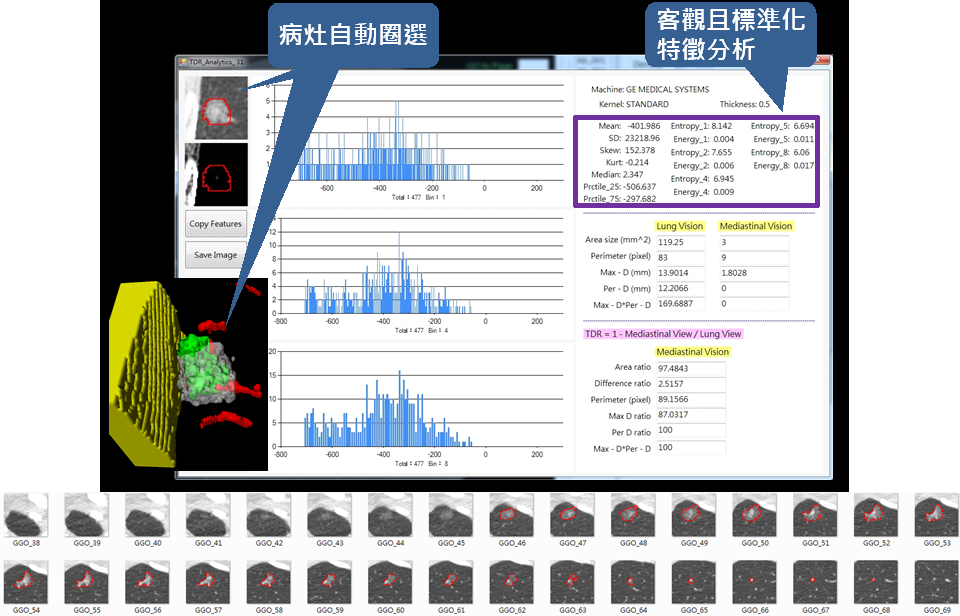
1. Established a computer-aided analysis platform (CAD) for computed tomography images, and applied it to surgical patients with lung cancer or suspected lung cancer. Preliminary results showed that by combining the mean value and entropy value of CT nodule density, CAD can effectively distinguish lung carcinoma in situ, minimally invasive lung adenocarcinoma, and invasive lung adenocarcinoma.
2. Clusters of circulating cancer cells in blood of advanced disease could predict patient prognosis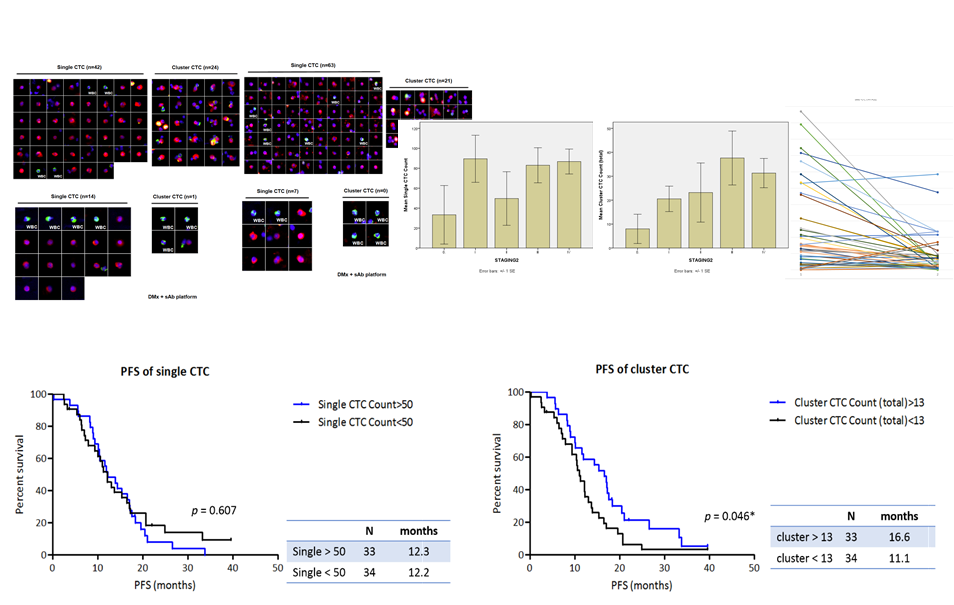
3. Through regular monitoring of changes of cfDNA EGFR mutations level, it is possible to predict the time of progression during EGFR-TKIs treatment.

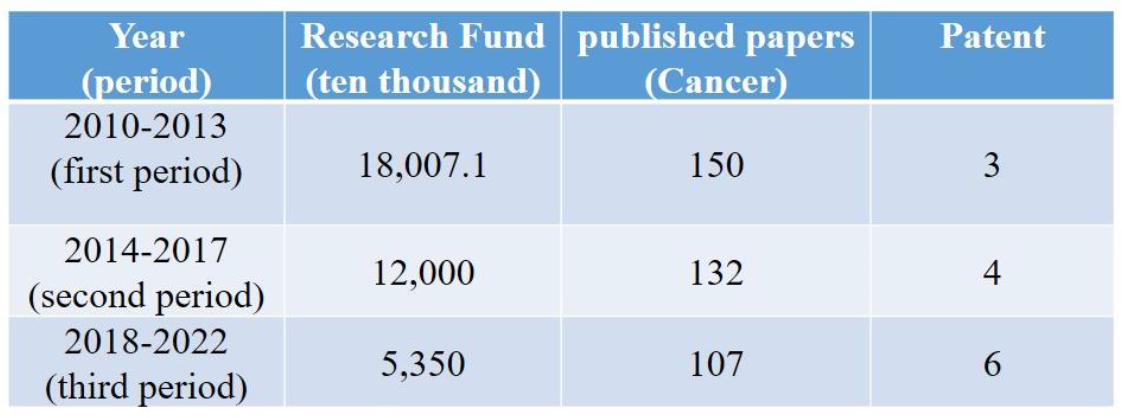
Research results and funding statistics
Chueh-Chuan Yen
Chief, Center of Excellence for Cancer Research, Taipei Veterans General Hospital
Mei-Whey Hung/ Min-Chuan Hsu
Tel. (02)28757409/(02)55688100
e-mail: vghtpecrc@gmail.com
Last Modified: