Kidney transplantation
- Living donor者
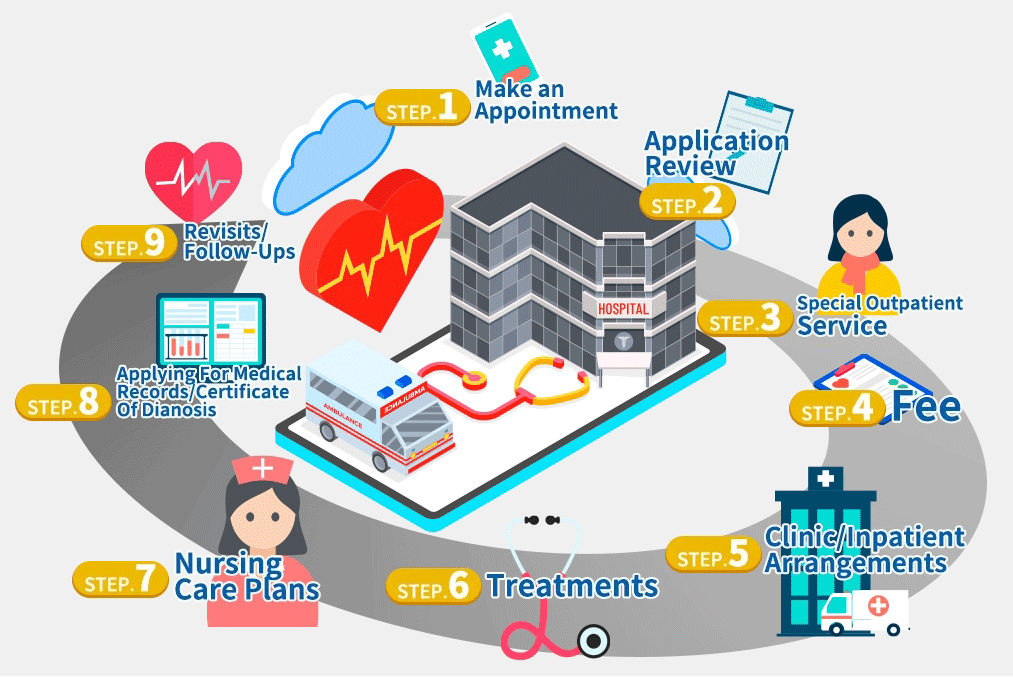
Application review
The requirements of being a living kidney donor
1.The donor has to be at least 20 years old, healthy, and related by blood within 5 generations to the recipient, or to be the spouse of the recipient. According to the law, the donor needs to be in the marriage with the recipient for at least 2 years, having children with the recipient, or married to the recipient a year before the recipient is diagnosed having the need of kidney transplant.
2.Both kidneys function normally.
3.The donor does not have the following diseases: diabetes, high blood pressure and tuberculosis. The donor does not have history of malignant tumors or infectious diseases which are forbidden by law such as AIDS.
4.The donor donates his/her kidney of his/her own free will and pure motivations.
5.The blood type requirements of the donors
The same or compatible blood types of the donor and the recipient is the first priority. For instance, a blood type O donor can donate his/her kidney to the recipient of any blood types; a blood type O recipient can only receive the kidney from a blood type o donor; a blood type AB recipient can receive the kidney from the donor of any blood types. Under some special circumstances, it is allowed to have kidney transplant surgery with incompatible blood types. However, the survival rate of the transplanted kidney is lower, and the chance of rejection is higher.
Blood type-incompatible kidney transplantation
Treatments before ABO-incompatible kidney transplantation
1.Reducing the remaining blood type antibody: plasmapheresis and giving IVIG
2.Reducing the active of B cell: giving rituximab 375 mg/m2 7-10 days before the surgery
3.Reducing the active of T cell: giving tacrolimus, mycophenolate mofetil; with/without corticosteroid, basiliximab, alemtuzumab, antithymocyte globlin. And proper antibiotics to prevent infection
After these medicine treatments, according to the researches, ABO-incompatible kidney transplantation can lead to the similar results as ABO-compatible cases, including survival of the patient, the function of the graft, the change of rejection and infection. However, for those whose blood type antibody titer is higher than 1:512, the allograft rejection rate is still higher than ABO-compatible transplant. It indicates that they have higher incidence of chronic rejection. Therefore, the patient whose blood type antibody is higher needs to take the medicine and follow up more carefully to have the best result.
Clinic/inpatient
It takes 4-8 weeks to complete the evaluations step by step. If the donor is in good medical, social, psychological and metal health, the surgery will be arranged after our medical ethics committee approves the application.
Step. 1
Blood test:
( 1 )the function of the kidneys and the liver, blood counting, anti-HAV, anti-HBV, anti-HCV, blood type, syphilis, AIDS, hemostasis and tissue matching
( 2 ) Image check: chest X ray, abdominal ultrasound, breast ultrasound, mammography (female)
(3)Other: electrocardiography, urinalysis and urine cytology
Step. 2
( 1 )Blood test: Virus antibodies, tumor indexes, thyroid function and tuberculosis
( 2 )Image check: kidney CT and comprehensive renal function test (ERPF)
Step. 3
( 1 )Mental status examination
( 2 )Evaluation of social workers
( 3 )Blood lymphocyte cross matching test
Review of medical ethics committee
According to the Human Organ Transplant Regulations of Taiwan, the comprehensive information both of the donor and the recipient need to be reviewed by our medical ethics committee. The surgery will be arranged with its approval.
Treatments
Surgery approaches and procedures
A living kidney donation is performed under general anesthesia. Therefore, during the surgery, you will not feel anything. In order to detecting the central venous and blood pressure, a central venous catheter will be inserted in the right part of your neck, and an artery catheter will be inserted in your upper limb. The use of a foley is also necessary.
There are 2 approaches of the surgery: open surgery and laparoscopic surgery:
1.Open surgery is performed in the abdomen or the back abdomen. First step is separating the kidney artery, kidney vain and proximal ureter, at the same time, separating the kidney from the surrounding tissues. Afterwards, the doctor will remove the whole kidney and preserve it in organ preservation solution. After the kidney is completely removed and the bleeding is stopped, the doctor will stitch the incision.
2.A laparoscopic surgery offers smaller incisions, equally successful outcomes, less pain, shorter recovery time and less days staying in hospital. First, the doctor will infuse carbon dioxide in the abdomen or the back abdomen, and then make 3 small incisions. Through these incisions, the doctor can insert the instruments and a camera in the donor’s body to perform the surgery. In the end, the kidney will be removed from the incision of the lower quadrant of the abdomen. There will be $80,000-$100,000 NTD at the donor’s own expense.
Nursing care plans
The risks and complications of living donors
1.The remaining kidney of a healthy donor, who received a full evaluation before the surgery, performs its normal function. According to long term follow-up studies, the life expectancy or the incidence of chronic kidney diseases (uremia) of the donors is the same with people who have not had the surgeries.
2.There are 2 approaches of the surgery: open surgery and laparoscopic surgery, taking 4-6 hours each. The donor needs to stay in the hospital for 5-7 days. The wounds will be different depending on the type of the surgery. According to the statistics, the death rate of living kidney transplant is lower than 1/1,000.
3.The incidence of complications is 8%-16%, including infection (2.4%), pneumothorax (1.5%), major bleeding and in need of bleeding control (<1%), pulmonary embolism (1%) and ureter stricture and urinary incontinence (2-10%). In the long-term change of 10 years after the surgery, the glomerulus filtration of the remaining kidney shows no significant difference, but around 30% of the donor may minor proteinuria or high blood pressure
Revisits/follow-ups
After discharged from hospital, you need to visit your doctor to follow up your condition once a week in the beginning. After stabilizing, you may visit the doctor once every 2 weeks or a month. During the visits, you will need to take blood and urine tests to measure the kidney function.
最後更新: