Liver transplantation
- Recipients
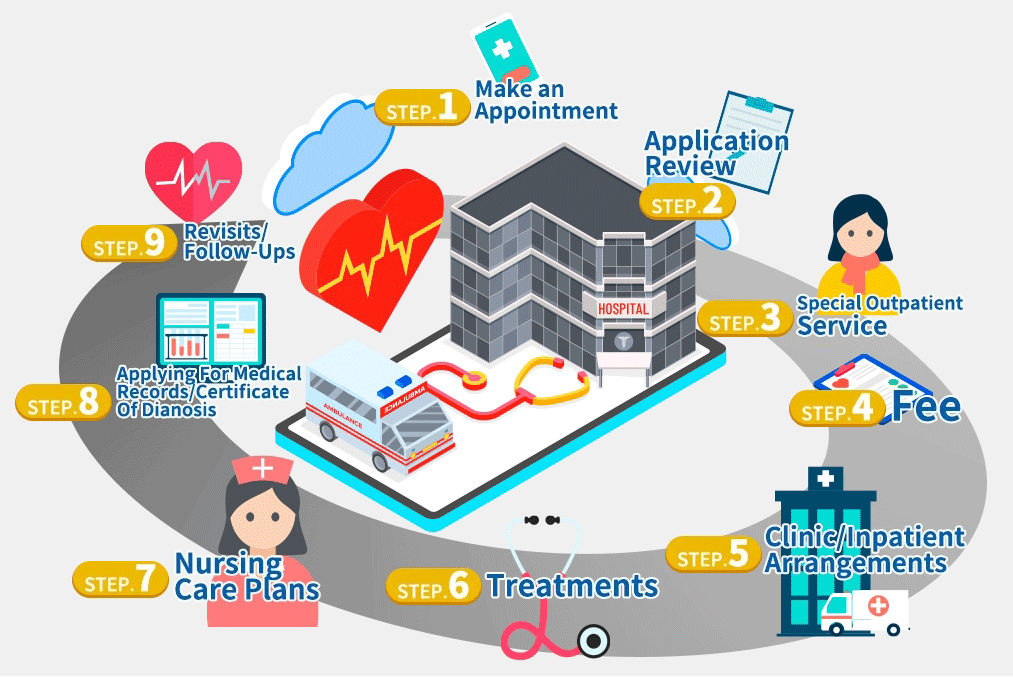
Qualification review
Living liver transplantation is another option for patients who have the end stage liver diseases (except end stage liver cancer) to save or extend their lives. Most end stage liver failure patients are suitable for liver transplant unless the patient has other contraindication, such as septicemia, aids, malignant tumor of outer liver, severe cardiovascular disease, drug addiction or alcohol addiction.
The assessment is to measure the suitability of patient and to provide important information for the patient.
Examinations and assessments
1.medical records review
2.blood type and tissue matching
3.Regular blood, biochemical, urine and stool tests
4.Virology examination
5.infection assessment
6.breast x ray and abdominal ultrasound (or abdominal CT)
7.Optional gastroscopy
8.electrocardiogram
9.psychiatrist consultant
10.social worker consultant
11.nutritionist consultant
If patients are also elders or having diabetes, they need to take further cardiac examinations, such as cardiac ultrasound or systolic function. Elder women need to take breast and cervix examinations. Elder men need to take prostate examinations and bladder function examinations if having difficulties of urination. Oral health is also important. If you have cavities, you need to take treatments immediately. Otherwise, they may become the cause of transplant infections.
Clinic/inpatient arrangements
We will arrange the following living transplant examinations:
1.Blood tests:
Blood type, functions of liver and kidney, hepatitis ABC, the virus quantity of hepatitis BC (NTD $3,000 each, self-pay), syphilis, AIDS, blood counting, hemostasis, tissue matching, autoimmune system, virus check, tumor indexes, PIVKA II (for liver cancer patients, NTD $1,750, self-pay), Human T-lymphotropic virus (HTLV-I/HTLV-II), thyroid function, arterial blood oxygen, latent tuberculosis infection (NTD $,2OOO, self-pay)
2.Image check:
All patients: liver transplant CT, 3D image synthesis (NTD $3,OOO, self-pay), abdominal blood vessel ultrasound and chest x ray
Liver cancer patient: chest CT, whole body bone scan and positron emission tomography (if needed, NTD $40,OOO, self-pay)
Female: Breast ultrasound and mammography
3.Consultations
Psychology division: evaluating if the patients are in good medical, social and psychological conditions.
Cardiology: cardiac ultrasound for evaluating if the cardiac function is suitable for the transplant surgery
Colon and rectal surgery division: colonoscopy and proctoscopy for evaluating if the rectum, colon or ileum having malignant tumors
Gynecology and obstetrics: pap smear test and ultrasound for evaluating if having malignant tumor
4.Other: electrocardiography, urinalysis and urine cytology
5.Examinations of stress Free endoscopic and colonoscopy are at the patients’ own expenses, NTD $4,000 for each, NTD $6,000 for together.
Treatments
A living liver donation is performed under general anesthesia, therefore, during the surgery, you will not feel anything. In order to detecting the central venous and blood pressure, a central venous catheter will be inserted in the right part of your neck, and an artery catheter will be inserted in your upper limbs. The use of a bladder Foley catheter for monitoring urine output is also necessary. The surgery is performed in abdomen. The liver with cirrhosis will be removed from the incision that looks like a Mercedes-Benz logo. Besides the ill liver, part of the arteries and vein connecting with the ill liver, common hepatic duct and the whole gallbladder will also be removed. Then, place the new liver in the abdomen. The resource of new liver may be a deceased donor or a closed-relative living donor. The new liver will be connected with your liver veins, inferior vena cava, hepatic portal vein, liver arteries. When they are all matched, the new liver will receive blood flowing through. Then, the doctor will connect the new liver with your bile ducts and small intestine, and then create a new bile drainage duct. However, the new liver does not come with the gallbladder. Sometimes, it is necessary to remove the gallbladder or ligate the left kidney vein during the surgery. After the surgery, the doctor will place some drainage tubes in the abdomen for the bleeding drainage and observing biliary leaks or biliary bleeding.
Nursing care plans
1.To preventing the rejections damage the new liver, you need to take anti-rejection medicines for the rest of your life. The anti-rejection medicines are also known as immunosuppressive drugs. Taking the medicines may lead to some complications, including higher chance of having cancers and infections, damage of kidney and nerves and metabolic disease (hyperglycemia, hyperuricemia and hyperlipidemia). You need to regularly test the concentration of medication and certain indexes of blood.
2.You may have psychological or metal issues due to the surgery and the anti-rejection medications. With these conditions, you may take counseling or medical treatments.
Revisits/follow-ups
After discharged from hospital, you need to visit your doctor to follow up your condition once a week in the beginning. After stabilizing, you may visit the doctor once every 2 weeks or a month. During the visits, you will need to take blood tests to measure the liver function and the drug level of the anti-rejection medication. You may also need image study (ultrasound) every 3~6 months.
最後更新: